Drivingdreams.In
Bringing together People who Drive their own Dreams!
Discogenic Pain Syndrome
http://www.chirogeek.com/IDD%20Page/IDD.html
Discogenic Pain Syndrome
 Just because that disc of yours looked normal on MRI, does not mean that it is eliminated as a source of chronic lower back pain. This is because that innocent looking disc, especially if it is black in color, [132] may be harboring a pain-generating "tear" inside of it, and these "annular tears" have the capability to produce dreadful and agonizing chronic low back pain which can be referred to as a Discogenic Pain Syndrome or Internal Disc Disruption. As the name implies, discogenic pain is pain that arises from the disc itself, secondary to tears within the annulus fibrosus.
Just because that disc of yours looked normal on MRI, does not mean that it is eliminated as a source of chronic lower back pain. This is because that innocent looking disc, especially if it is black in color, [132] may be harboring a pain-generating "tear" inside of it, and these "annular tears" have the capability to produce dreadful and agonizing chronic low back pain which can be referred to as a Discogenic Pain Syndrome or Internal Disc Disruption. As the name implies, discogenic pain is pain that arises from the disc itself, secondary to tears within the annulus fibrosus.
Why hasn't my doctor mentioned discogenic pain syndrome as possible cause of my chronic low back pain? Frankly, it is probably because he or she just is not that familiar with the different causes of chronic low back pain.
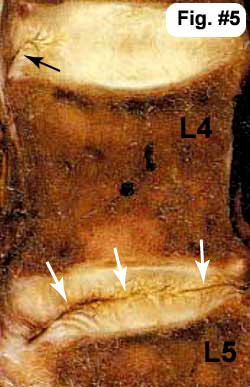
Fig.#5 The white arrows are pointing to a full thickness annular tear (or an internally disrupt disc) within the L4/5 disc that in this case completely bisects the disc (there are many different flavors of annular tear– see the annular tear page). Note also that the disc above (the L3/4 disc) has a small tear in the outer fibers of the annulus (black arrow) that has not made it (yet) into the middle of the disc. This type of tear is called a 'rim lesion'.
What is the "prevalence" (how often does it occur within the population) of torn-disc-related low back pain (discogenic low back pain or Internal Disc Disruption? Although the research on this subject is not particularly thorough, one landmark paper demonstrated that 30% to 50% of people with chronic low back pain suffered from these disc tears, a condition which can also be called internal disc disruption (IDD). [2]
Before I continue, it's very important to understand that not all cases of internal disc disruption cause chronic low back pain, and the mechanisms that make some annular tears symptomatic and others not, remains elusive. I personally believe it has something to do with the individual's unique immune system and ability to generate inflammation. Nevertheless, this is a fairly controversial diagnosis as some researchers just don't believe in, although others (including Bogduk {a very well respected and conservative, award-winning spinal anatomist and researcher) are adamant about its existence.
Is the diagnosis of internal disc disruption new? No. In fact it has been around for at least 50 years, for at that time (1986) H.V. Crock told members of the International Spine Society that 'internal disruptions' within the architecture of the disc could result in back pain as well as lower limb pain, independent of nerve root compression. [9] it was he that coined the term IDD.
How Does Internal Disc Disruption Occur?
Internal disc disruption occurs when the posterior annulus (whose job is to hold the highly pressurized nucleus pulposus in the center of the disc) tears (usually from the inside out) which in turn allows nucleus pulposus to escape from the confines of the disc's center and push into the outer, nociceptively innervated (filled with pain-generated nerve fiber) regions of the disc.
How does the tear start in the first place? It is believed that these tears develop from (#1) arduous activity, such as engaging in a heavy/physical job, or participating in heavy contact sports; (#2) severe single-event trauma (e.g., a motor vehicle accident or a slip and fall); and / or (#3) a genetic predisposition for tearing (the annulus was built with faulty/weak material that is quite easily torn).
In order to understand how IDD may cause pain, you will need to know some basis disc anatomy. If you are a little shaky on disc anatomy, please visit my disc anatomy page before you proceed [here].
Quick Disc Anatomy Review
 Fig.#4 demonstrates the normal lumbar disc anatomy: Here, in this over-head view, we have the nucleus pulposus (pink) surrounded by the the stronger annulus fibrosus (green). Normally, the annulus fibrosus is strong enough to contain or corral the pressurized nucleus pulposus and keep it from escaping (squirting) outward. Of particular interest to the upcoming discussion are the tiny 'Sinuvertebral Nerves Endings' (yellow poke-a-dots). These tiny nerve fibers, which are embedded within the posterolateral substance of the outer 1/3 of the annulus fibrosus, are known to both initiate and carry the perception of pain into the spinal cord. From there, these pain signals are carried upward to the sensory cortex of the brain. (386-388, 439).
Fig.#4 demonstrates the normal lumbar disc anatomy: Here, in this over-head view, we have the nucleus pulposus (pink) surrounded by the the stronger annulus fibrosus (green). Normally, the annulus fibrosus is strong enough to contain or corral the pressurized nucleus pulposus and keep it from escaping (squirting) outward. Of particular interest to the upcoming discussion are the tiny 'Sinuvertebral Nerves Endings' (yellow poke-a-dots). These tiny nerve fibers, which are embedded within the posterolateral substance of the outer 1/3 of the annulus fibrosus, are known to both initiate and carry the perception of pain into the spinal cord. From there, these pain signals are carried upward to the sensory cortex of the brain. (386-388, 439).
ADVANCED: The pain pathways (how the degenerated disc tissue pain gets from the disc to the brain) for discogenic pain are still very controversial and may not function as traditional anatomy has taught us. Traditionally, pain signals that originate in the nerve roots adjacent to the disc or within the disc itself move from that root, into the corresponding DRG and then into the spinal cord. However, some new research suggests that pain signals from the lower lumbar discs (L5 and L4) are (at least in part) detoured up the sympathetic nerves (i.e., gray ramus communicans) and into the upper lumbar DRGs - especially at the L2 level. (11, 259, 260) Clinically, in some patients it then would be possible for patients with L4 and L5 disc problems to have L1 or L2 dermatomal pain (groin and anterior thigh pain).
How & When Does An Annular Disc Tear Become Painful?
In order for the tear to become painful, it must lead to (or occur in) the posterior one-third of the disc, which of course (I hope you studied your disc anatomy) is where the pain-carrying nerve fibers of the sinuvertebral nerves live. Although controversy, the exact mechanism of pain is two-pronged:
#1) it is believed that "evil" pro-inflammatory biochemicals (like the cytokines TNF-a, IL-1, IL-6), which are known to occur in high concentrations within degenerated disc tissue, will leak and soak into the nociceptors (pain switches) of the sinuvertebral nerve, which in turn triggered the nociceptors to fire signals of pain to the brain. This is known as a chemical irritation of the nociceptors. Furthermore, now in information can start in the adjacent tissue which in turn perpetuates the irritation of these nociceptors.
#2) The full thickness tear will also destroy the normal biomechanics of the disc which changes the point of maximum weight-bearing from the center of the disc to the posterior part of the disc which is where all these inflamed nociceptors are. So now, every time the patient twists, turns and bends at the waist, the already inflamed and irritated nociceptors are mechanically irritated, which also upsets them and triggers them to send pain impulses to the brain.
Autoimmune Reaction?
There is some evidence that the actual nucleus pulposus cells which leak from the center of the disc into the region of the nociceptors (i.e., outer one third of the posterior and posterolateral disc) results in an autoimmune inflammatory process, because these cells have never been seen by the body's immune system before.
 In Fig. #3 the disc has ripped through or "disrupted" and has allowed nuclear material (pink) to escape into the outer and sensitive 1/3 of disc (i.e. the annulus fibrosis). The sinuvertebral nerves (yellow dots) in contact with this degenerated nuclear material have become inflamed (red dots) and irritated, which in turn causes pain signals to 'fire off' to the dorsal horn of the cord and then to the brain, which causes the patient to feel pain. Some patients even suffer a referred type pain (discogenic sciatica) down the lower limb(s), yet they have no traditional compression of the adjacent nerve roots. [jump to tutorial]
In Fig. #3 the disc has ripped through or "disrupted" and has allowed nuclear material (pink) to escape into the outer and sensitive 1/3 of disc (i.e. the annulus fibrosis). The sinuvertebral nerves (yellow dots) in contact with this degenerated nuclear material have become inflamed (red dots) and irritated, which in turn causes pain signals to 'fire off' to the dorsal horn of the cord and then to the brain, which causes the patient to feel pain. Some patients even suffer a referred type pain (discogenic sciatica) down the lower limb(s), yet they have no traditional compression of the adjacent nerve roots. [jump to tutorial]
HISTORY OF INTERNAL DISC DISRUPTION: (IDD)
IDD was first described by Crock in 1970 (8) and again in 1986 (9). Specifically, it was then described as a ‘disruption' of the internal architecture of the disc without signs of disc protrusions or without positive signs for nerve root compression’.
In his 1986 presidential address, Dr. H. V. Crock told members of the international spine society that internal disruptions within the architecture of the disc could result in back pain and even lower limb pain without the presence of spinal nerve root compression (9). He termed this entity ‘Internal Disc Disruption’ or IDD.
In 1995, a 'Dream Team' of well respected and Volvo Winning researchers (Schwarzer, Aprill, Derby, Bogduk) set out to test and further develop Crock’s theory of IDD and convincingly calculated the prevalence (frequency) of IDD in patients with chronic low back pain. (2) The study also attempted to determine if traditional examination findings and/or specific patient symptoms could be predictive of the diagnosis of IDD. By following the strict criteria specified by the ‘International Society for the Study of Pain in its taxonomy’ (21), these investigators calculated the prevalence of IDD to be between 30% and 50% with a 95% confidence limit. They also concluded that neither traditional examination findings nor patient symptoms could predict whether or not a patient had IDD. Unfortunately, it looks like the controversy over diagnostic procedure, provocation discography, remains the only way to confirm the diagnosis of IDD.
The Critics of Internal Disc Disruption
The theory of IDD as a source of chronic back pain is not without its critics. In 2003, Lee et al. reviewed the research on IDD from 1985 through 2000, (10) although the papers review were mostly geared toward radial tears and HIZ. He summarized that of the 13 research papers on IDD, there was not much agreement on what constituted the diagnosis of IDD. What the authors did agree upon, however, was that patients with IDD had concordant low back pain upon provocative discography and a completely normal neurological examination (i.e., there were no deep tendon reflex changes, no loss of sensation, and no muscle atrophy or weakness). Other signs of IDD, which include the MRI presence of a high intensity zone (HIZ), significant disc degeneration (a black disc on MRI), and a history of trauma to the lumbar spine, were not universally agreed upon by the experts.
Based on their review of '15 years worth of research', Lee et al. concluded that “IDD is not real, but a hypothetical disease”. This Korean group further stated the following; “Our personal view is that IDD is a doctor-made disease, that is, an iatrogenic disc disorder, which may lead to an unconventional invasive operations (referring to the IDET procedure and Lumbar Fusion).” [10] Furthermore, Lee felt that because the diagnosis was so dependent upon the 'subjective input' from the patient during discography, that the diagnosis should be thrown out completely!
IMHO: Lee, who is way out of his usual area of research on this subject, is going to be criticized for making such aggressive statements against the theory of IDD, which has been accepted by the 'North American Spine Society' (21) and the 'International Society for the Study of Pain in its Taxonomy' (21)! For the typical non-mentally compromised chronic pain patient, the diagnosis of IDD can be made with a reasonably degree of medical certainty by using the criteria that the International Society for the Study of Pain in its Taxonomy have adopted (Here) for the criteria.
Internal Disc Disruption: Other Research
Although controversial (436), discogenic pain secondary to IDD is thought to be responsible for a substantial number of chronic back and leg pain cases where obvious nerve root compression is absent/lacking. [132, 2] In fact the famous multi-time Volvo Award Winning author, professor Nikolai Bogduk MD, believes IDD is the "most common cause of chronic low back pain" (1,2) and may be often over-looked by the treating physician." (132).
Quality scientific research has demonstrated that 30% to 50% of all chronic back pain is caused by the radial annular tears of IDD, [2] and often presents (62% of the time according to Ohnmeiss et al.) as back pain and/or pain down the lower extremity. [6]
The theory on how the annular tears within the annulus cause chronic low back and leg pain remains fairly speculative and contraversial. However, the available research seems to indicate that evil biochemicals called "cytokines" may leak from the degenerated nucleus pulposus onto the nociceptive fiber that lives within the posterior and posterolateral annulus fibrosus, which in turn sets up a vicious cycle of inflammation – pressure buildup – nociceptive stimulation (pain). [105,115,116,123,124,131]
Recently, it has been demonstrated that IDD was the causative factor in about three-quarters of severely acute nonspecific low back pain patients. More explicitly, in 2005 Hyodo et al (16) performed MRIs and discography on 55 patients who all suffered severe, immobilizing, non-specific low back pain without sign of neurological deficit. In 73% of these patients, a full thickness non-epidurally leaking annular tear was identified on discography that responded to fluoroscopic lidocaine irrigation (a powerful anesthetic) by instantly 'stopping' the patient's perception of severe pain. (16) The aforementioned experiment strongly advocates that full thickness annular tears – or IDD – are a major cause of severe acute non-specific low back pain.
Why do annular tears affect patient in the forth and fifth decade of life?
Why the pressure buildup? Onik goes on to explain [304] that the intervertebral disc may be considered an osmotic system and because of a breakdown in macromolecules during the fourth and fifth decades of life, the number of particles in the intervertebral disc increase, which in turn causes a concomitant rise in osmotic pressure secondary to an influx of fluid, which in turn increases the intradiscal pressure. In order to relieve the pressure, annular fissures develop that result in symptomatic annular tear and disc protrusion and PAIN.
THE DIAGNOSIS: Discography & Gadolinium-DTPA Enhanced MRI
The 'International Society for the Study of Pain in its taxonomy’ (21) has adapted the following set of criteria for diagnosing IDD: ►) no visible disc herniations may be seen on MRI or CT; ►) during provocation discography injection of the suspect disc with contrast, a recreation of patients 'exact' back and/or leg pain must occur (353,9); ► injection the disc above or below the suspect disc must be non-painful; this acts acts as a 'control disc' or normal disc; and ► a grade 3 or 4 radial anular fissure must be demonstrated on CT discography (2,351,352,355).
 Provocation discography, which may actually further damage the disc, should ONLY be attempted if the chronic pain patient can no longer live with their pain syndrome and is contemplating IDET, SED, DiscTRODE, interbody spinal fusion or ADR. Furthermore, their Oswestry better be at least a 50! (Oswestry)
Provocation discography, which may actually further damage the disc, should ONLY be attempted if the chronic pain patient can no longer live with their pain syndrome and is contemplating IDET, SED, DiscTRODE, interbody spinal fusion or ADR. Furthermore, their Oswestry better be at least a 50! (Oswestry)
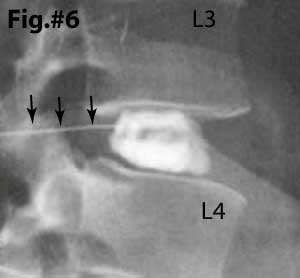
The 'Gold Standard' in making the diagnosis of IDD is a very painful and invasive test called 'Provocation Discography' with follow-up CT discogram. There are two components to provocation discography: the first is an attempt by the doctor to 'provoke' or 'cause' the patient to feel their 'usual' pain (concordant pain) by pressurizing the disc with a contrast material. Note: in Fig.#6 the center of the disc is being filled with contrast material (white). If you look closely, you can see the fine 'white' needle (black arrows) entering the posterior of the disc. This (fig. #6) represents a normal disc that 'holds' the dye within the nucleus and does not demonstrate any anular tearing.
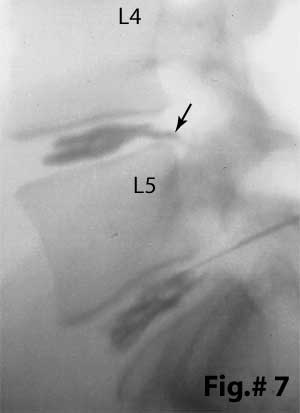 Fig.#7, on the other hand, demonstrates two completely disrupted discs: The contrast material (black in this photo) has NOT been contained within the center (nucleus) of the disc. This time, it has clearly leaked through internal 'disruptions' within the posterior annulus of the L4/5 and L5/S1 disc. In fact, the L4/5 disc has been completely disrupted and it leaking contrast material directly into the epidural space (black arrow). The latter situation is called a Grade 5 anular tear or Grade 5 IDD. (learn about the Dallas discogram naming system and the different degrees of disc disruption here about half way down the page.) This situation may indicate big trouble, especially if you are one of unfortunates who are 'sensitive' (allergic) to those leaking biochemicals (cytokines), for the delicate posterior neural structures 'dwell' adjacent to the posterior of the disc and may become inflamed and/or damaged from this leakage. More explicitly, substance like TNF-alpha, IL-1, IL-6, NO, Phospholipase A1 may stimulate some form of 'attack' within the nerve root and ultimately lead to permanent nerve (axon) death. Neuropathic pain may be spawned.
Fig.#7, on the other hand, demonstrates two completely disrupted discs: The contrast material (black in this photo) has NOT been contained within the center (nucleus) of the disc. This time, it has clearly leaked through internal 'disruptions' within the posterior annulus of the L4/5 and L5/S1 disc. In fact, the L4/5 disc has been completely disrupted and it leaking contrast material directly into the epidural space (black arrow). The latter situation is called a Grade 5 anular tear or Grade 5 IDD. (learn about the Dallas discogram naming system and the different degrees of disc disruption here about half way down the page.) This situation may indicate big trouble, especially if you are one of unfortunates who are 'sensitive' (allergic) to those leaking biochemicals (cytokines), for the delicate posterior neural structures 'dwell' adjacent to the posterior of the disc and may become inflamed and/or damaged from this leakage. More explicitly, substance like TNF-alpha, IL-1, IL-6, NO, Phospholipase A1 may stimulate some form of 'attack' within the nerve root and ultimately lead to permanent nerve (axon) death. Neuropathic pain may be spawned.
MRI Identification: Gadolinium-DTPA Enhanced MRI
Although provocation discography with CT discography is the "gold standard" when it comes to making the diagnosis of symptomatic IDD, the procedure itself can inflict damage upon the disc and "spawn" degenerative disc disease (30-34,530). As an alternative, the use of gadolinium (contrast) enhancement may be considered. Gadolinium-DTPA, which is injected into the blood stream during the MRI, will "light-up" the granulation tissue that forms within a healing/healed full thickness annular disc tear.
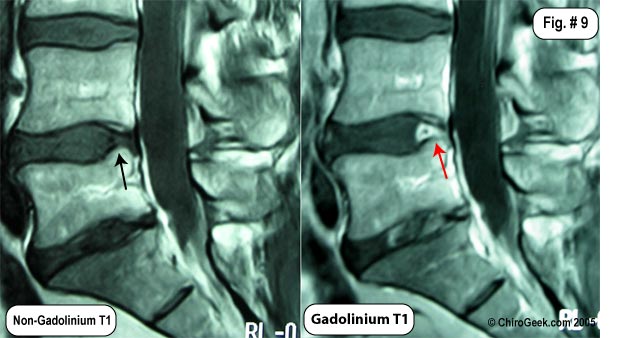 Fig.# 9: The MRI images to the left demonstrates how gadolinium will "light-up" a healed anular tear. Note the L4 disc shows no sign of posterior disc tearing (black arrow); however, after the administration of gadolinium during the MRI, the same T1 image demonstrates the remains of the massive annular tear (red arrow) I suffered back in 2002.
Fig.# 9: The MRI images to the left demonstrates how gadolinium will "light-up" a healed anular tear. Note the L4 disc shows no sign of posterior disc tearing (black arrow); however, after the administration of gadolinium during the MRI, the same T1 image demonstrates the remains of the massive annular tear (red arrow) I suffered back in 2002.
The gadolinium also high-lights continued swelling/granulation tissue within my L5 disc over 1 year post microdiscectomy. No disc herniations are noted.
The HIZ phenomenon also give us a clue that Internal Disc Disruption might be involved in the patients pain syndrome although this T2-weighted MRI finding is highly controversial. For more information, visit my HIZ page.
The Internal Disc Disruption Tutorial
To begin this tutorial, lets look at what a normal disc looks like from the underneath view (axial):
 In Figure #4, the basic anatomy of the disc is shown. First note the gelatinous and hydrated nucleus pulposus that is corralled (held in place) by a tough and fibrous annulus fibrosus. The posterior longitudinal ligament (PLL) (blue) is a strong fibrous ligament that courses the entire length of the spine and is tightly bound to the posterior central region of the annulus. It is because of this ligament, that many disc herniations occur in the paracentral region where it is not located.
In Figure #4, the basic anatomy of the disc is shown. First note the gelatinous and hydrated nucleus pulposus that is corralled (held in place) by a tough and fibrous annulus fibrosus. The posterior longitudinal ligament (PLL) (blue) is a strong fibrous ligament that courses the entire length of the spine and is tightly bound to the posterior central region of the annulus. It is because of this ligament, that many disc herniations occur in the paracentral region where it is not located.
Particularly important for this tutorial is to note the presence of pain-carrying nerve fiber embedded within the posterior disc. These are called the sinuvertebral nerves and are thought to be responsible for the chronic low back pain associated with annular tears.
It is extremely important to understand that, unlike the rest of the avascular disc, the outer 1/3 of the annulus fibrosus, anterior dura and the PLL are innervated with (full of) tiny nociceptive C-fibers (pain carrying nerve fiber from the sinuvertebral nerves) that, if irritated, have the potential to cause severe PAIN and DISABILITY (4,55,56).
Internal Disc Disruption: Of How It Typically Occurs
*If you don't understand axial disc anatomy, I strongly recommend that you visit the Disc Anatomy Page in order to get a basic understanding and then returned here—I'm going to assume you know it.
 Typically, the first step in the IDD process is for the disc to become brittle and weak from degenerative disc disease (DDD) because such a weakness may allow trauma or reparative trunk motion to start a tear in the inner annulus (figure 2, black arrow). However, full thickness annular tears can also begin in the periphery of the disc and then work their way in. [30-34,530]
Typically, the first step in the IDD process is for the disc to become brittle and weak from degenerative disc disease (DDD) because such a weakness may allow trauma or reparative trunk motion to start a tear in the inner annulus (figure 2, black arrow). However, full thickness annular tears can also begin in the periphery of the disc and then work their way in. [30-34,530]
Figure 2, is a cartoon of a disc that has degenerated, become brittle, and developed both circumferential annular tears (white arrows) and a radial annular tear (black arrow). Because the radial tear is confined within the inner one-third of the annulus, we called this a grade I annular tear. Grade I annular tears are typically not painful (recall from your disc anatomy lesson that the pain-carrying sinuvertebral nerves are only located in the outer one-third of the annulus) but can develop into a painful full thickness annular tear (a.k.a., grade III) with continued activity or additional trauma.
 In the figure left, the disc has in fact developed a full thickness annular tear (red arrow) which has allowed nucleus pulposus to come in contact with the nociceptive fibers of the sinuvertebral nerves.
In the figure left, the disc has in fact developed a full thickness annular tear (red arrow) which has allowed nucleus pulposus to come in contact with the nociceptive fibers of the sinuvertebral nerves.
How could this full thickness tear be painful? The first reason has to do with biomechanics. As you may recall from the disc anatomy page, when the nucleus is no longer contained to the center, the closed hydraulic system is ruined. Specifically, axial load will now be transmitted directly over the posterior portion of the disc, which is right where the nociceptors are. Therefore, as the theory goes, you get a mechanical irritation of the nociceptors, which in turn creates an inflammatory process (depicted by red nociceptors adjacent to the annular tear). The second reason is because degenerative nuclear material contains some very evil biochemicals called cytokines and others (TNF-alpha, NO, PLA-2, Metalloproteinases, IL-6, PGE-2, Substance-P, Calcitonin gene-related peptide) which now have direct access to the nociceptors, and may start an inflammatory process. Many believe it is this double whammy that creates the horrible low back pain associated with full thickness annular tears of the posterior disc. [287]
*There is also an autoimmune theory, which I happen to be a believer in, that goes like this: because the cells of the nucleus pulposus came to being after birth, and because the nucleus is completely avascular and therefore not exposed to the body's immune system, the cells of the nucleus may be considered foreign. Therefore, if these foreign invaders break out of the nucleus and enter the vascular outer one-third of the annulus (which is also the location of the nociceptors), the body's the immune system may attack and create an inflammatory reaction in the outer annulus, which in turn will trigger the pain-producing nociceptors.
 Can a full thickness annular tear cause radicular pain (a.k.a., lower extremity pain, or sciatica)? The short answer is, yes! However, this can only occur if the full thickness annular tear breaks through the final layers of annulus and begins to "drizzle or leak" the evil biochemicals from the disc, onto the adjacent traversing and/or exiting nerve root. (figure 8)
Can a full thickness annular tear cause radicular pain (a.k.a., lower extremity pain, or sciatica)? The short answer is, yes! However, this can only occur if the full thickness annular tear breaks through the final layers of annulus and begins to "drizzle or leak" the evil biochemicals from the disc, onto the adjacent traversing and/or exiting nerve root. (figure 8)
Figure 8 depicts just such a scenario: the full thickness annular tear is now leaking biochemicals, as well as small molecules of nuclear material, which in turn have soaked into the exiting and traversing nerve roots of the sciatic nerve and started a wicked inflammatory process, resulting in radicular pain.
Internal Disc Disruption: The Available Treatment Options
|
Warning: These recommendations are for Educational Purposes ONLY and should never be substituted or take the place of an examination by your own medical doctor! Do NOT implement any of these courses of treatment without the approval of your medical doctor.
|
IDD is a very, very tough condition to treat, especially since the diagnosis is fairly controversial to begin with and many primary doctors have never even heard of it. Conservative care is ALWAYS the first form of treatment! If this fails then provocation discography is indicated before proceeding to the more aggressive treatment options but your Oswestry should be in the 50s. Here are the current (7-28-04) treatment options available of IDD:
|
TREATMENT OPTIONS FOR IDD (in order) for 2013 |
|
|---|---|
| Conservative Care, Medication & Mother Nature: |
80% to 90% of all IDD sufferers will obtain satisfactory relief from their pains by just hanging in there and using conservative measures and allowing mother nature to do her thing. However, it's very easy for the patient to become frustrated by the fact that IDD often takes many months (12-24 months, depending on how much DDD is present) to heal. I would NEVER recommend a patient rushing into a decompressive fusion (or even SED) until they have waited at least 18 months (preferably 24 month), unless serious medical complication occur (i.e., loss of bowl & bladder control, progressive neurological deficit, or severe intractable pain). Give mother nature a chance. Another trick is to figure out a way to get that heart rate of yours up in an aerobic zone, without flaring up. This will enhance blood flow to the disc and annular tear, which in turn should help with the healing process by increasing nutrient delivery and waste removal. Also, get plenty of sleep, which is where diurnal change allow the disc cells to get fed and allows for waste removal. |
|
Fusion: |
If conservative care and other less invasive surgeries fail, and you just cannot take the pain and disability any longer, lumbar interbody fusion is your last change. The most important part of this treatment is to find a doctor who knows what the hell they are doing. The three major techniques are anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF). Visit my Fusion Page to learn more about the techniques and read our recently published paper (TLIF for DPS) to see what our results were for the treatment of this condition (i.e., discogenic pain syndrome, aka: internal disc disruption (IDD), or isolated disc disruption(IDR)). |
References:
Comment
-
Comment by Driving Dreams International on April 3, 2016 at 7:58pm
© 2026 Created by Driving Dreams International.
Powered by
![]()
You need to be a member of Reflexology to add comments!